Tetralogy of Fallot: A Parent’s Guide
Congenital Heart Defect
Tetralogy of Fallot is a congenital heart defect that affects the structure of the heart and changes the way blood flows through the heart and to the lungs.
It is a rare type of congenital heart defect and babies born with it will require heart surgery soon after birth.
Key Points:
- Tetralogy of Fallot is a congenital heart abnormality, and the word tetralogy refers to the four defects that characterise the condition.
- It is the most common type of cyanotic heart disease, representing 5-7% of all diagnoses
- Babies born with Tetralogy of Fallot will need to have surgery conducted after they are born or during infancy to repair the defects

What is Tetralogy of Fallot (TOF)?
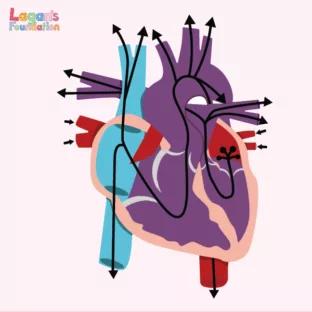
Tetralogy of Fallot (TOF) is a congenital heart condition made up of four different heart defects:
- Ventricular Septal Defect (VSD) – A defect where a hole forms between the bottom two chambers (ventricles) of the heart.
- Overriding Aorta – The aorta sits between the right and left ventricle, over the VSD. In a normal heart, the aorta comes off the left ventricle.
- Pulmonary Stenosis – The pulmonary valve is more narrow than normal and doesn’t open properly. This makes it harder for the right ventricle to pump blood to the lungs, causing the baby to have low oxygen levels.
- Right Ventricular Hypertrophy – The right part of the heart has to work harder, causing the right pumping ventricles to get thicker.
How is Tetralogy of Fallot diagnosed?
During pregnancy, tests can be conducted by a doctor to check if your baby has any heart problems. However, some problems may not be present until the baby is born.
During pregnancy
A prenatal ultrasound can be used during pregnancy to check for any complex heart defects. This test will show if your baby’s heart is not shaped correctly. If this is found, you will usually be scheduled for a foetal echocardiogram to help gather more information about your baby’s heart.
A foetal echocardiogram is a special type of ultrasound used by paediatric doctors to look closely at your baby’s heart and surrounding blood vessels. Once your baby is born, a cardiologist will assess your baby’s heart again with an echocardiogram to confirm the diagnosis.
Foetal MRI’s can also be used, which is a type of imaging that gives a more detailed picture of your baby’s organs. It can be used to find problems with the heart or lungs.
After birth
After your baby is born, an echocardiogram can be used to get a closer look at your baby’s heart. However, there are other ways in which TOF can be diagnosed after birth.
Heart catheterisation is a test to measure pressure in the heart. It can take pictures of the heart and open narrowings with a balloon or small metal coil, called a stent. This process is conducted while your baby is under anaesthesia.
Another way to diagnose TOF is by using a cardiac MRI. This test uses radio waves, magnets and a computer to make a detailed image of the heart and the surrounding blood vessels. Cardiac MRI’s can provide detailed information on the type and severity of the heart disease.

There are several other tests that doctors can conduct to find out if the baby has TOF, including:
- Pulse Oximeter – This involves a small sensor being clipped onto the baby’s fingertip, toe or ear to measure how much oxygen is in the blood. This is a common test for many newborns to check their oxygen level is normal before they go home. This is non-invasive and does not hurt.
- Electrocardiogram – This test records the electrical activity of the heart.
- Chest X-rays – This test takes an image of the chest.
How does Tetralogy of Fallot affect the heart?
As we’ve discussed, Tetralogy of Fallot is made up of four different heart conditions. However, you may be wondering how these conditions actually affect the heart.
- A Ventricular Septal Defect is a hole in the separating walls (septum) between the two lower chambers (ventricles) of the heart. The septum normally acts as a barrier that prevents oxygen-rich and oxygen-poor blood from mixing.
When there is a VSD, the two types of blood can mix. This can lead to either too much or too little blood flowing into the lungs. Children born with TOF usually have a large VSD.
- An overriding aorta means that the artery that carries oxygen-rich blood to the body is out of place and sits above both ventricles, instead of just the left ventricle.
This allows some oxygen-poor blood to flow into the aorta and out to the body instead of the pulmonary artery, which would normally take it to the lungs and collect oxygen.
- Pulmonary Stenosis is the narrowing or thickening of the valve that connects the right ventricle to the pulmonary artery (the blood vessel that carries oxygen-poor blood from the heart to the lungs).
With pulmonary stenosis, the heart has to work harder than a normal heart to pump blood to the lungs. There is also less blood travelling in the lungs because the pathway is narrower, resulting in less blood becoming oxygen-rich. Sometimes babies with ToF are born with pulmonary atresia, in which the pulmonary valve is completely sealed off.
- Right Ventricular Hypertrophy is a thickening of the muscular wall of the right ventricle. The thickened wall can contribute to the blocking of blood flow through the pulmonary valve, which allows blood from the heart to flow into the lungs.
What are the symptoms of Tetralogy of Fallot in children?
One of the most common signs of Tetralogy of Fallot is cyanosis, which refers to a bluish-purple colour to the skin. Healthy babies sometimes have bluish skin around their mouth or eyes, but their lips and tongue look pink. However, babies born with ToF will typically have blue lips and tongues in addition to bluish skin.
Sometimes, a baby with ToF will have sudden episodes of deep cyanosis during crying or feeding. This is known as ‘hypercyanotic spells’ or ‘Tet spells’.
The ToF cough
Another main symptom is the ‘ToF cough’, which is a loud, barking cough that affects many children with Tetralogy of Fallot (ToF) and other conditions, such as oesophageal atresia (OA) and tracheo-oesophageal fistula.
It’s caused by tracheomalacia, a condition where the trachea (windpipe) is floppy. The cough is caused by the child coughing through the floppy section of the trachea, which makes an unusual sound.
Although the ToF cough can sound alarming, it’s usually not serious and doesn’t necessarily mean the child is sick. It can get worse when a child has a cold or other respiratory problems. The sound of the ToF cough may continue into adulthood.
Other signs and symptoms to be aware of include:
- Heart murmurs
- Fussiness
- Tiring easily
- Difficulty breathing
- Heart palpitations
- Fainting
- Clubbing (the skin or bones around fingertips are widened or rounded)

What causes Tetralogy of Fallot?
The specific cause of Tetralogy of Fallot is not known; however, in some cases, genetics are thought to be the main reason. For example, babies born with Down Syndrome or DiGeorge syndrome are more likely to have Tetralogy of Fallot.
Babies of mothers who have Rubella or other viral illnesses during the pregnancy are also at a higher risk of ToF.
Other pregnancy-related risks that are thought to be associated with ToF include poor nutrition, alcohol use, poorly controlled diabetes and the mothers age. External environmental factors are also thought to increase the chance of ToF, such as air pollution.
How is Tetralogy of Fallot treated?
Tetralogy of Fallot can be treated through open-heart surgery soon after the baby is born or later on during infancy. This will depend on the baby’s health and weight and the severity of the defects and symptoms.
The two options for surgery are:
- Complete Repair – The surgeon widens the passage between the right ventricle and pulmonary artery to improve blood flow to the lungs. The Ventricular Septal Defect is patched to stop the mixing of oxygen-rich and oxygen-poor blood.
These repairs also fix the two other defects of the overriding aorta and right ventricle hypertrophy. This is because the right ventricle doesn’t have to work as hard to pump blood into the lungs and the thickness of the walls will decrease. The patched VSD prevents oxygen-poor blood from flowing into the aorta.
- Temporary or Palliative Surgery – Minor repairs can improve blood flow to the lungs. This is usually only done when a baby is too weak or small to have full surgery. Your baby’s surgeon will create a secondary route for blood to travel to the lungs for oxygen by placing a small tube, a shunt, between a large artery branching off the aorta and the pulmonary artery.
Once the baby is stronger, they can then be considered for the full repair surgery.
Most babies who have Tetralogy of Fallot repaired do very well after surgery, however, they will need regular follow ups with a heart specialist throughout their whole life.
What is the life expectancy of a child with Tetralogy of Fallot?
It can be difficult to predict the life expectancy of a child with a Tetralogy of Fallot. However, data suggests that those who have had it repaired will live up to 30 – 40 years after complete repair.
Knowledge about the survival rates is made difficult since recent advances in surgical techniques and intensive care management have had a positive effect on the survival rates early on and late after surgery.
Are there other conditions associated with Tetralogy of Fallot?
Most babies who are born with Tetralogy of Fallot don’t have any other conditions, but some do. Some babies may have a syndrome called ‘22q11 deletion’ or DiGeorge syndrome, where a small piece of genetic material is missing from their DNA. Others may have syndromes such as Down’s Syndrome.
If your baby is diagnosed with ToF, your doctor will discuss with you the options of having a test to find out if they have chromosomal abnormalities. If the ToF is diagnosed before birth, these tests can be carried out before your baby is born.

![Understanding Total Anomalous Pulmonary Venous Return [TAPVR]](/wp-content/uploads/2025/04/Understanding-Total-Anomalous-Pulmonary-Venous-Return-FI-312x312-c-default.jpg)